Huntington's disease care pathway collaborative project.
This project was a collaborative partnership with Surrey Heartlands Health and Care Partnership (SHHCP), Kent Surrey Sussex Academic Health Science Network (KSS AHSN), Roche Products Ltd. and the Huntington’s Disease Association.
About the project
The project took place between July 2021 to January 2022.
A co-production/co-design approach was taken with stakeholders from SHHCP, St George’s Hospital, local health and social care professionals, Roche, Huntington's Disease Association, patients, families and carers impacted by Huntington's. Engagement included surveying patients, families and carers across England and Wales to understand where current care services worked well, and two Surrey specific co-design events. Learning from this helped shape a service delivery model for Huntington's disease patients in Surrey, and led to the successful proposal to develop and recruit to a new Huntington's disease coordinator post.
Download the report
Project aims
The project aimed to build on existing services to develop a service model that is fit for purpose and provides equitable care for Huntington's disease patients, family members and carers.
The service model will be introduced for the care of patients with Huntington's disease, their family members and carers residing in Surrey.
The need for a service model
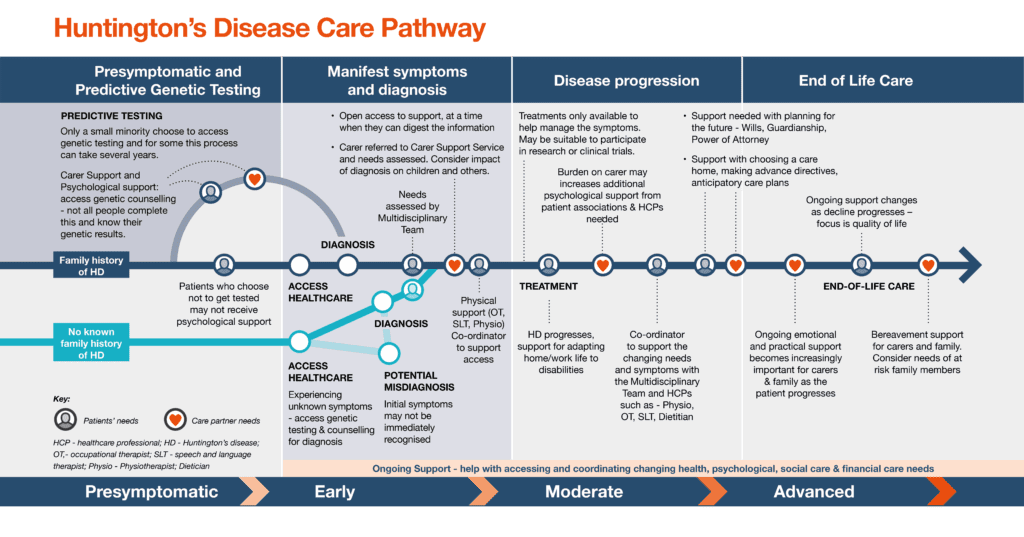
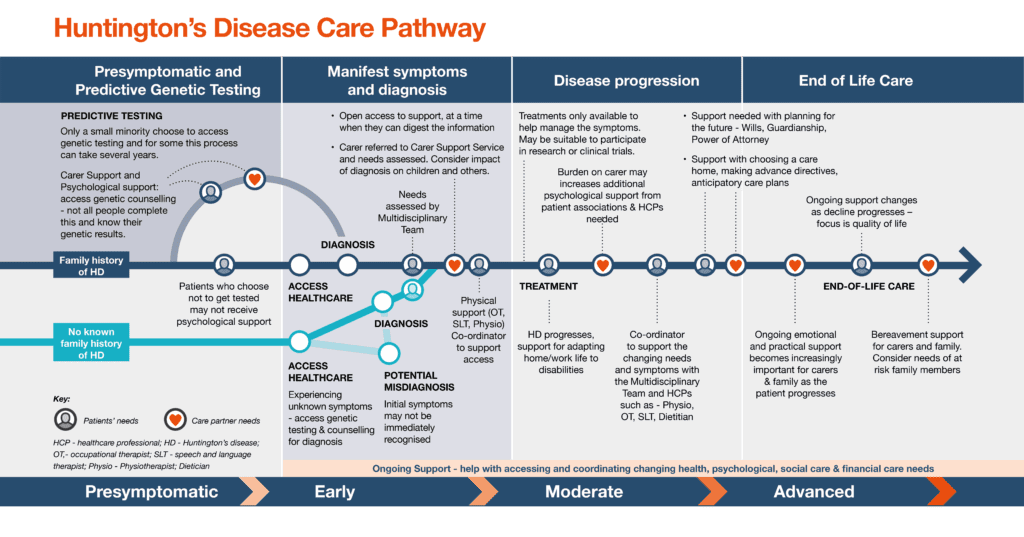
Huntington’s disease is a rare, inherited, neurodegenerative disease, with onset usually in mid-adult life. It progressively affects a person’s everyday functions with particular impact on movement, thinking, personality and behaviour.
Huntington's disease has a devastating impact across generations, due to the inherited nature of the disease but also due to the effect on family members and carers living with affected individuals. For every parent with Huntington's, there is a 50% chance for each of their children of inheriting the condition. Huntington's disease can show genetic anticipation with an earlier age of onset of symptoms in subsequent generations. This leads to significant worry and stress for those with Huntington's disease, and their relatives who are seeing the effect that it has on their loved one and deciding whether to test for the gene themselves.
Whilst there are medications and interventions that can help control some of the effects of the disease, there is currently no way to prevent, slow or stop disease progression. Huntington's disease is ultimately fatal and progresses relentlessly from the appearance of symptoms to loss of functional capacity and disability, with a median survival of 15 years from the onset of motor symptoms. Huntington's symptoms typically start between the ages of 30 and 50, with prodromal (pre-diagnosis) subtle changes in thinking, mood, and behaviour.
Challenges and solutions
Communication
Challenges
- Lack of coordinated support across services/organisations – acute, mental health teams, community teams, palliative care teams
- Lack of appropriate pathways between neurology and mental health services and social care
- Main challenges for patients are mental health issues both cognitive and psychiatric. Different phases of the illness will need different care provision
- Patients have complex care needs which can result in rapid deterioration
- Social workers not able to link to Psychiatrist or Neurologist
- Person with Huntington's disease not linked in with any specialist care centre/clinic e.g National Hospital for Neurology, Queens Square London or St George’s
- Lack of specialist support (or not knowing who/where to signpost them to) when patient in the “maintenance” phase
- Lack of specialist support (or not knowing who/where to signpost them to) when behavioural changes/ challenging behaviour phase starts
Solutions
- Care Co-ordinator (a potentially joint role with another neurological disease or across a wider geographical area)
- MDT approach across the whole system
- Review service specifications for current local services and adapt them to ensure Huntington's disease patients get equitable services.
- Joint or polyclinics between all services involved in the patients care
- Trigger points to recognise the palliative phase
- Referral to Huntington's Disease Association built into pathway
- Referral to a regional or national Huntington's disease Specialist Clinic on diagnosis and a 6-12 monthly follow up or earlier should clinical symptoms need reviewing
Support
Challenges
- Lack of mental health support e.g you have access to mental health advisor who gives advice to GP but then patient are not under the umbrella support of mental health team so not supported and treated as a one-off episode
- Not getting right pharmacological management in respect of mental health and wellbeing
- No local support groups/networks for patient/carers/family members
- Brigette Trust neurological support group won’t accept Huntington's disease patients
- Knowing how to access continuing health care funding
- Input provided by appropriate Huntington's disease specialists for continuing health care funding requests
Solutions
- Multidisciplinary team (MDT) approach
- Care co-ordinator
- Neuro psychology input for Huntington's patients in conjunction with other neuro conditions
- Review service specification for current local services and adapt it to ensure Huntington's disease patients get equitable services
- NHS to consider funding Huntington's disease amongst some of the existing local support groups across Surrey
- Signposting to Citizens Advice for funding support built into the pathway
- A checklist for continuing healthcare is completed when a patient deteriorates from their normal baseline/ functional level and that change is irreversible. This should be completed by someone who knows the patient.
Care homes
Challenges
- Lack of guidance/guidelines especially for those Huntington's patients who are care home residents with clear directives of not wishing to go to hospital
- Uncertainty around symptom control measures to put in place for care home residents with Huntington's disease e.g. feeding and medication adherence
- Limited choice of residential care due to complex needs/challenging behaviour of patients
- Care home or care provider say they might accept someone but once seen and accessed the patient they are refused
Solutions
- Care co-ordinator who knows the patient and supports them across the disease progression, including in a care home
- Peer agreed guidelines/guidance on how to care for Huntington's disease patients with input from Neurologists and Geneticists and palliative care
- Identify barriers as to why care providers feel they can’t meet Huntington's patients' needs
- Commission a training/awareness programme
Knowledge and awareness
Challenges
- Lack of understanding of complexities of needs amongst health (including mental health) and social care professionals
- Lack of knowledge and understanding of Huntington's disease by clinicians on the continuing health care assessment panels
- Lack of training for paid carers
Solutions
- Care co-ordinator who can support professionals who don’t have specialist knowledge of Huntington's disease
- Commission a training and awareness programme
Project outcomes
Providing Huntington's patients, family members and carers with coordinated multidisciplinary (MDT) holistic care as they progress along the stages of this disease. Huntington's disease is a complex condition that requires a “Care Coordinator” role to facilitate the multi-disciplinary team (MDT) approach of care provision to address the constantly changing needs of patients and family members living with this degenerative disease. The service will deliver these aims by establishing defined models of care with robust shared/network care arrangements where appropriate.
A long-standing problem for those affected by Huntington's disease is that their disease crosses the boundaries of medical, psychiatric and social problems. This complex care should be supported by a care coordinator who can help and support the patient and careers to navigate the care they need.
Download the service model
Dr Nayana Lahiri, Consultant Geneticist, St George’s Hospital and Trustree, Huntington's Disease Association said:
“The project sought to identify the unmet needs for care for families with Huntington’s disease. It was successful in bringing together multiple stakeholders from a number of different backgrounds across the breadth of care needs in Huntington’s disease and highlighted a need for improved partnership working and co-ordination of care. KSS successfully navigated a complex area and drew together multiple strands to create a workable service specification and identify roles that could serve as a model for improved care and partnership working.”
Download the report
Huntington's disease Care Coordinator role
Identifying the correct care pathway and signposting patients is a unique challenge which Care Coordinators can play a vital role in overcoming.
Care Coordinators provide expert advice on care, along with practical and emotional support, helping those with neuromuscular conditions to manage their condition throughout their lives. They also help coordinate the care of patients outside clinics and can provide support to non-specialist health professionals in the community either directly or by signposting those professionals to appropriate specialist services.
The role ensures people living with Huntington's disease have a local expert on their care needs in the local community, who can give advice about appropriate referral pathways to patients, GPs and community services. They will be able to support patients to ensure appropriate support is offered between specialist centres, and community teams.
The focus of this role will be to provide holistic support and advice to Huntington's disease patients, their carers and family members living across Surrey. The post holder will work closely with individuals living with Huntington's and their families to co-ordinate clinical care and improve overall quality of life.
Job purpose
- To coordinate the provision of community services for people with Huntington's, working in partnership with patients and carers, health and social care colleagues, and voluntary and private sector agencies.
- To provide specialist input to patients with Huntington's disease and their carers, to enable them to manage their condition and live as independently as possible.
- To develop regional multi-disciplinary team (MDT) meetings for complex case discussion, outreach and training.
- To develop appropriate, individualised management plans.
- To develop and maintain robust links between neurological clinics in secondary care and the community service.
- To work to reduce the rate of admissions and length of hospital stays for patients with Huntington's disease, by working as part of the wider multi-disciplinary team (MDT).
- To assist in maintaining a condition register to aid commissioning.
- To have in depth clinical experience at specialist level and extend and maintain this knowledge base by attending relevant courses/meetings as agreed by the line manager.
- To act as an expert resource and provide Huntington's-specific training to health and social care professionals and support staff of all grades involved in caring for people with Huntington's disease.
- To keep and maintain accurate clinical records.
Dimensions
- To work in a variety of community settings which may include the patient’s own home/Care/ Nursing Home/clinic setting.
- To lead the delivery of a specialist Huntington's disease care service across a variety of clinical and other settings including inpatient, outpatient clinics, domiciliary visits and hospice admissions.
- Act as a speciality expert, leading case management and coordination of the wider multidisciplinary team to meet both clinical and service delivery goals.
- To provide a ‘single point of contact’.
- To maintain clinical databases.
- Provide clinical education, training, supervision and support to other staff and students within speciality area.
- To manage own specialist workload effectively within the clinical and professional policies of the Organisation.
- To deliver audit, quality improvement and the coordination of research studies.
- To ensure that the service successfully meets national, local and departmental quality and clinical standards.