People living with Huntington’s can be more at risk of weight loss for a number of reasons.
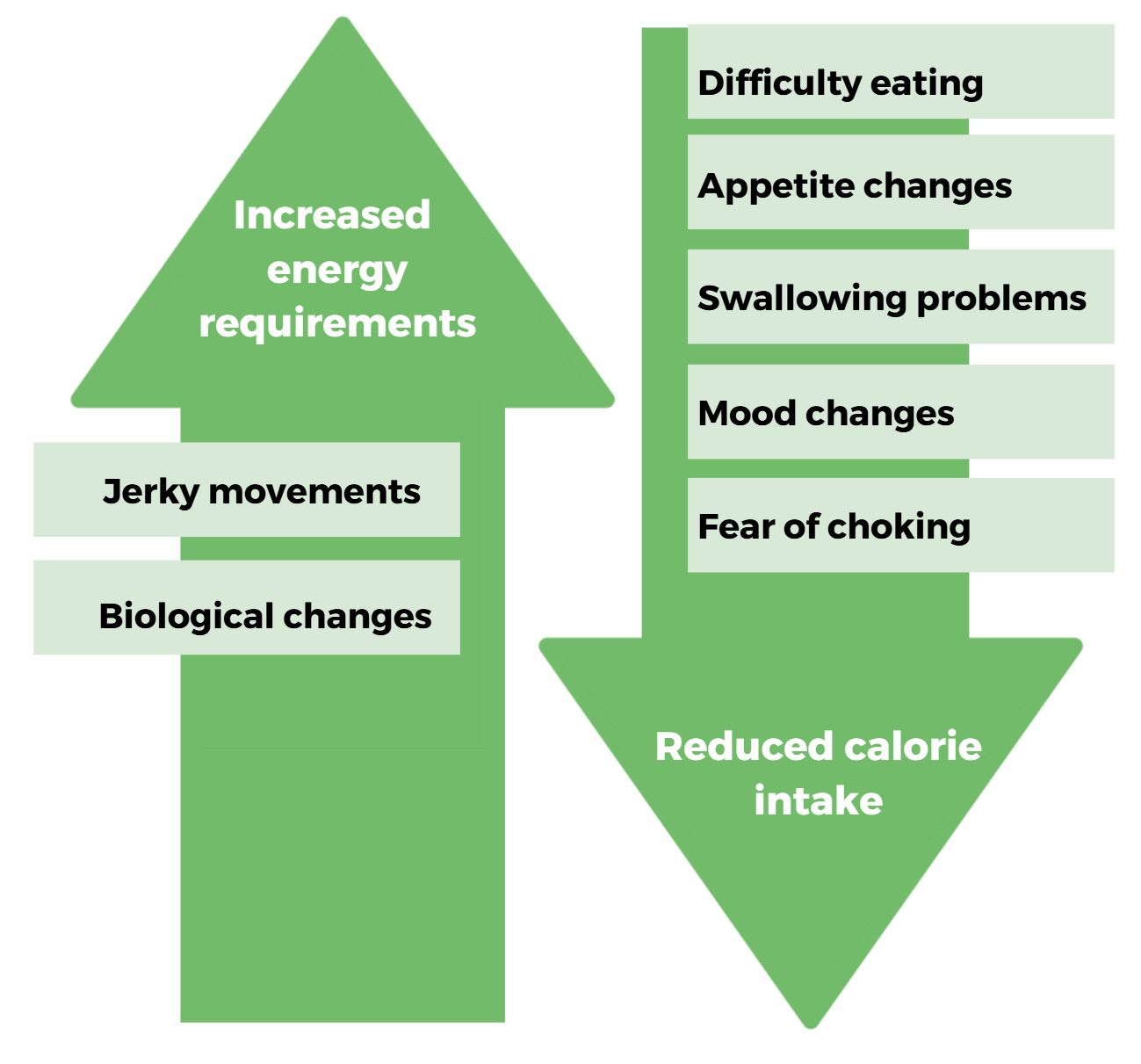
Weight loss may slowly occur during the early stages of Huntington’s disease and may go unnoticed for a while. As Huntington’s progresses and more symptoms appear, people often find it more difficult to maintain their weight and to prevent significant unintentional weight loss. People with Huntington’s usually need to eat a diet which is higher in calories than normal in order to minimise weight loss. However, it is more common to see somebody using up more energy, whilst also decreasing food intake. This is known as the nutrition gap.
Tips on how to avoid weight loss
- Instead of three main meals a day it may be easier to try smaller meals and snacks every two to three hours.
- Prioritising food which is high in calories and protein means that even if a small amount of food is managed, vital nutrients can still be absorbed.
- Similarly, using full fat milk or cream as an accompaniment to cereals, puddings and drinks is an easy way to increase protein and calcium intake.
- Adding extra butter, cheese or mayonnaise to savoury meals, and syrup, sugar, jam or honey to sweet snacks, is a good way to add calories to a meal.
- Drinking with a meal can decrease appetite, so should be monitored or avoided altogether.
- Regular snacks like biscuits, chocolate and crackers should help keep weight up.
- Fortified drinks based on full fat milk, such as Complan, are commercially available and can be added to meals to increase energy and protein intake.
- Keeping a food diary can help a health professional identify where there may be areas that need attention. Details like portion size and the way that a meal is cooked can be incredibly helpful.
What to do if food is not enough?
Food may not be enough and if weight loss continues regardless of what is being eaten, speak to a GP to discuss the unintentional weight loss. Bringing along a five day food diary and indication of the total weight lost over the last three to six months may help the conversation. If the GP identifies there is a risk of malnutrition, they may make a referral to a dietitian.
What to expect from a dietitian
A dietitian will carry out a nutritional assessment which focuses on how Huntington’s disease is impacting nutritional status. A nutritional care plan will then be created and carefully monitored to ensure nutritional requirements are met. If someone is at risk of malnutrition or are malnourished, the dietitian may advise on the use of prescribed medical nutrition for the dietary management of disease-related malnutrition and/or dysphagia.
Medical nutrition
Medical nutrition products are specialised foods designed to meet the needs of those living with a medical condition, recovering from an illness or operation, of those who have become weak over time. They are often referred to as Oral Nutritional Supplements (ONS) or Food for Special Medical Purposes (FSMP). Medical nutrition products are usually prescribed by a healthcare professional and must be used under medical supervision.
Oral nutritional supplements
Oral nutritional supplements are available in a variety of formats and styles, including shakes, juices, yoghurts, and desserts, as well as a variety of flavours to suit different taste preferences.
Tube feeding
Tube feeding is a way of getting a body the nutrition it needs. It provides a liquid form of nourishment that delivered into the body through a flexible tube. The nutrients are similar to those someone would get from normal food, and are also digested in the same way. It contains all the nutrients someone would need on a daily basis, including carbohydrates, protein, fats, vitamins, minerals and water.
Making the decision around tube feeding
For some people, a tube feed will be something they want; for others, it won't.
It is good to think about preferences early on in the disease. That way, you have the time to think about the pros and cons of tube feeding and what your preferences might be in the future. It's important that you record your preferences and that you let people involved in your care know your wishes.
Types of feeding tubes
There are two main types of feeding tubes which can be used. Nasogastric tubes (NG) are inserted through the nose and into the stomach. They are easier to fit as they do not require surgery, but they are generally used for shorter-term feeding.
Gastrostomy tubes - PEG (Percutaneous Endoscopic Gastrostomy) are inserted via a procedure called an endoscopy, which requires anaesthetic. If someone is going to need a feeding tube for a long time, a gastrostomy is likely to be the preferred option.
A healthcare professional will recommend what type of feeding tube is needed.
Tube feeding
Everyone has different nutritional requirements. The product a person requires will be tailored to their needs and will depend on weight, height, activity level, and if they can still eat and drink small amounts. A dietitian will be able to discuss and advise on the most appropriate product.
Eating well guide
You can read, download or share our full eating well guide from the link below.






